4-year-old female with spontaneous XLH*
Case summary
Findings/outcomes
- Although the patient was seen by multiple specialists, a conclusive diagnosis was not reached over a period of 13 months, after referral to an endocrinologist; the patient was subsequently followed by a nephrologist
Although XLH is primarily an inherited disease, 20% to 30% of cases arise spontaneously.1
Patient history
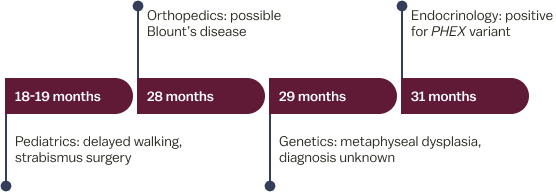
18-19 months: Pediatric evaluation
- 18-month-old female presented with leg bowing, wide-based gait, delayed walking, and poor growth; fear of climbing stairs
- X-rays: indicative of metaphyseal dysplasia
- Other clinical findings: strabismus, suspected to contribute to walking delay; underwent strabismus surgery
28 months: Orthopedic evaluation
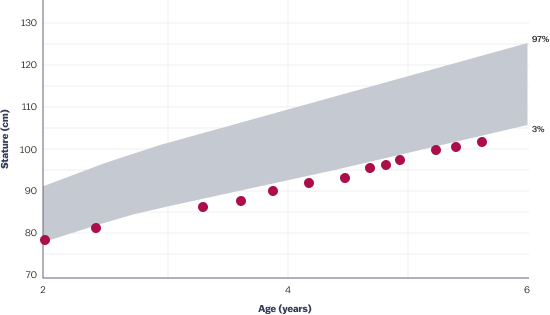
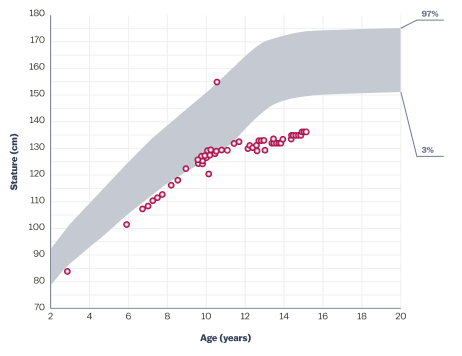
- Physical exam: short stature, height less than 5th percentile since age 15 months (See growth chart); worsened bowing and waddling gait
- X-rays: significant bilateral genu varum with mild beaking and sloping of the proximal tibial metaphysis; metaphyseal-diaphyseal angles of bilateral proximal tibiae measured 16 degrees; bilateral irregularity of the distal femoral metaphysis also noted; femoral heads were normally located
- Differential diagnosis: possible Blount’s disease, metaphyseal dysplasia, or physiologic genu varum
29 months: Genetics evaluation
- No family history of bone disease
- Suspected diagnosis: metaphyseal dysplasia
- Underwent genetic testing for Schmid metaphyseal chondrodysplasia and Shwachman-Diamond syndrome; results were negative for pathologic variants
- Diagnosis: unknown, referred to skeletal dysplasia clinic
31 months: Endocrinology evaluation
- Physical exam: bilateral genu varum
- X-rays: bilateral mild coxa vara, tibial varus (left greater than right) with metaphyseal irregularity and fraying of the distal femur, tibia, and ulna; metaphyseal widening at wrists
- Other findings: 2nd percentile for weight; 1st percentile for height (See growth chart)
Diagnosis
Hypophosphatemic rickets; positive for PHEX mutation; negative in parents—spontaneous X-linked hypophosphatemia
For patients with XLH, the diagnosis process can be long and laborious, and proper specialist referral can be key to early disease diagnosis.1,3
15-year-old female with spontaneous XLH*
Case summary
Findings/outcomes
- Bone health is an important consideration before growth plate closure
- Regardless of provider, asking about mental health was an important element of care
- Prevention of fractures and musculoskeletal health is critical
Symptoms of XLH are nonspecific when considered individually and vary between patients.1,3,4 Specialist referral is key to early diagnosis.
Patient history
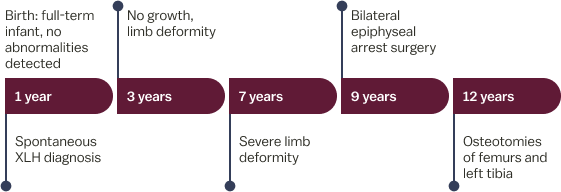
- Birth: full-term infant with no abnormalities detected
- 12 months: signs consistent with pain upon weight bearing; limping; bowed legs at 18 months
- Family history: unremarkable
- 30 months: X-rays – bilateral bowing with irregular and widened metaphyses at tibia and femur
- 34 months: key fasting laboratory findings (reference range‡)
- Serum phosphorus: 2.4 mg/dL (3.2-6.1 mg/dL)
- 25-hydroxyvitamin D: 39 ng/mL (20-50 ng/mL)
- Alkaline phosphatase: 512 U/L (ULN for ages 1 to 15 years ranges from 297-385 U/L)
- Serum calcium: 9.2 mg/dL (0 to 2 years: 9.0-11 mg/dL; 2 to 16 years: 8.4-10.3 mg/dL)
- Parathyroid hormone: 85 pg/mL (14-72 pg/mL)
Diagnosis
Spontaneous XLH
49-year-old male with hereditary XLH*
Case summary
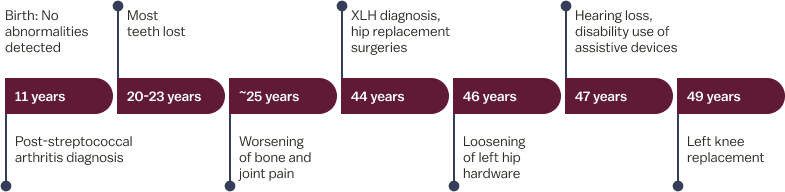
Findings/outcomes
- The patient was not diagnosed with XLH until age 44
- There is a spectrum for XLH, and the patient’s symptoms were not previously attributed to XLH
- Symptoms of XLH progressed throughout adulthood and had long-term impact. The patient:
- Required surgeries and developed worsening pain
- Required the use of assistive walking devices
- Developed hearing loss
- Needed dentures
It is important to diagnose XLH early, as the progressive nature of XLH leaves patients susceptible to short stature, fractures, limited function, and pain.1
Patient history
During childhood
- 6 years of age: humerus fracture from jumping off a moving truck
- Poor dentition of both primary and secondary teeth with multiple cavities and abscesses
- 11 years of age: reported “bone disease” due to chronic bone and joint pain
- Pediatrician diagnosed post-streptococcal arthritis
- Mild leg bowing; reported short stature compared to peers
Early to mid-twenties
- Lost most teeth by early twenties
- Acute worsening of bone and joint pain
- Suspected inflammatory arthritis
44 years of age
- Presented with acute exacerbation of chronic weakness and right hip pain
- Reported no previous diagnosis of rickets
- Family history
- Short stature and bowing of the lower legs in mother (height, 4’11”), three brothers, and two nieces; all had multiple fractures
- Physical exam
- Height, 5’3”; weight, 230 lbs
- Ambulating with assistance of a walker; knees in varus alignment
- Pain with internal rotation of hips (left worse than right); 4/5 motor strength in both proximal and distal muscle groups
- Poor dentition and missing most secondary teeth
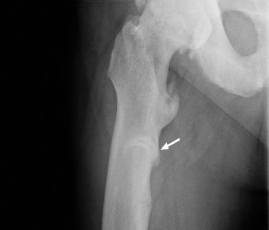
- X-rays
- Pelvis and hips: diffuse increased density of the bones, particularly in the iliac wings and lumbosacral spine; enthesopathic calcifications extending from the superior acetabular walls bilaterally (See X-ray 1); right subtrochanteric pseudofracture identified, which was incomplete along the medial cortical region (See X-ray 2)
- Femurs: pseudofractures in the subtrochanteric right femur and mid-left femoral diaphysis; healing stress fracture present in the medial cortex of the left femoral neck; enthesophytes and bilateral hip osteoporosis also noted (See X-ray 3)
- Laboratory findings (See Table)

44 years of age: Diffuse increased density of iliac wings and lumbosacral spine; bilateral enthesopathic calcifications extending from the superior acetabular walls.
44 years of age: Right subtrochanteric pseudofracture incomplete along the medial cortical region.
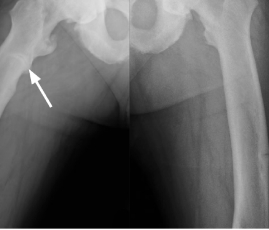
44 years of age: Pseudofractures in the subtrochanteric right femur and mid-left femoral diaphysis; healing stress fracture present in left femoral neck medial cortex; enthesophytes and bilateral hip osteoporosis.
Laboratory results
| Test (reference range unit‡) | 44 years (results) |
| Serum phosphorus (2.5-4.5 mg/dL) | 2.1 |
| 1,25(OH)2D (18-72 pg/mL) | 31 |
| 25(OH)D (20-50 ng/mL) | 33 |
| BSAP (6.5-20.1 mcg/L) | 39.2 |
| PTH (14-72 pg/mL) | 95 |
| Creatinine (0.7-1.2 mg/dL) | 0.83 |
| FGF23 (<180 RU/mL) |
73
|
The patient exhibited XLH signs and symptoms throughout childhood and young adulthood and was not diagnosed until his mid-40s.
Diagnosis
Hereditary XLH

 Français
Français