Family History
With known family history of XLH
XLH is inherited in an X-linked dominant pattern, so a positive family history of the disease supports the diagnosis. In a family with a history of XLH, screen other first-generation family members for XLH. This can help identify previously undiagnosed individuals.4,5
Without known family history of XLH
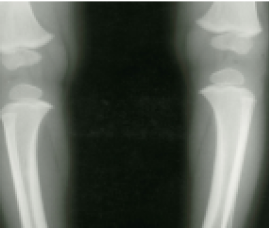
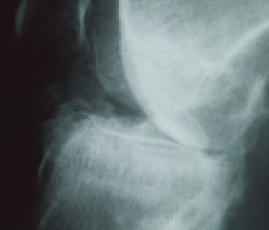
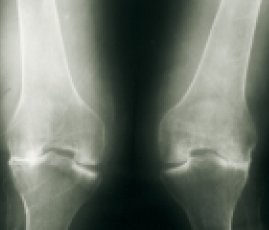
Since approximately 20% to 30% of XLH cases are spontaneous, it’s important to ask if your patient has a history of short stature, rickets, osteomalacia, osteoarthritis, and dental abscesses, all of which may indicate XLH.5
Biochemical findings
The following are predominant clinical findings in children and adults.
Evaluate age-normalized levels of fasting serum phosphorus for an accurate diagnosis. Low phosphorus levels and a low TmP/GFR ratio are the most relevant biochemical findings for XLH.4,5
| Biochemical Test | XLH |
| Fasting serum phosphorus |
|
| 1,25(OH)2D |
|
| 25(OH)D | Normal |
| TmP/GFR |
|
| ALP |
|
| Serum calcium | Normal |
| Urinary calcium |
Normal to decreased
|
| PTH | Normal or slightly up |
Confirmatory testing
In both children and adults, evaluating PHEX genetic variant status and FGF23 levels can help establish an accurate diagnosis for XLH.2,4,6
| Through a genetic analysis of the PHEX gene | By checking for elevated intact FGF23 levels |
Prioritize testing your patient’s serum phosphorus levels in addition to clinical, radiographic, and other biologic findings in order to diagnose XLH.
Preventing further complications
The progressive nature of XLH may lead to increasing clinical consequences over time.5 Early diagnosis of XLH in both adults and children may help prevent complications.1,4,5
Comprehensive care for patients
Symptoms of XLH are nonspecific when considered individually and vary between patients. Accordingly, patient care requires a comprehensive team of healthcare professionals and specialists to provide disease education for your patients.1
These specialists may include:1
- Endocrinologist
- Nephrologist
- General practitioner
- Pediatrician
- Physical therapists
- Orthopedic surgeon
- Rheumatologist
- Pain specialist
- Genetic counselor
- Dentist

 Français
Français